Exploring Funding and Resource Allocation Challenges in Healthcare Scaling
Addressing Budget Limitations in Healthcare Expansion
In the context of scaling healthcare in the UK, the challenge of budget constraints stands out as a significant hurdle. The National Health Service (NHS), a beloved institution, frequently finds itself wrestling with funding limitations that may stall or obstruct expansion initiatives. The complexity of the matter extends beyond merely securing financial resources; it involves the strategic allocation of funds to those areas that demand immediate attention. A comprehensive understanding of these financial constraints is imperative, as it can pave the way for the development of innovative solutions aimed at overcoming these challenges.
Healthcare providers are increasingly turning to alternative funding models, such as social impact bonds and public-private partnerships, as a means to alleviate financial pressures. In a system that emphasises free healthcare at the point of access, striking a balance between maintaining quality and expanding services becomes an intricate challenge. For instance, substantial investment in mental health services has been hindered by competing priorities within the system. The necessity for effective financial planning, which anticipates future demands and challenges, cannot be overstated.
However, the issue extends beyond mere financial resources; it encompasses the prudent deployment of available resources. In regions like Greater Manchester, the emphasis on integrated care systems aims to streamline services, ensuring that every pound spent serves a clear purpose. By analysing successful models from various healthcare trusts, we can glean insights on how to navigate these budgetary obstacles. Ultimately, a proactive budgeting approach, combined with a keen awareness of the current fiscal environment, can empower healthcare providers to adeptly navigate the complexities of financial limitations.
Strategically Prioritising Healthcare Services for Optimal Impact
Determining which healthcare services to prioritise for scaling is a task that necessitates keen judgement and a thorough understanding of public health needs. Within the UK, the NHS grapples with the challenge of prioritising services in a manner that maximises health outcomes while remaining financially sustainable. Service prioritisation evolves from being a mere strategy to a fundamental necessity when it comes to scaling healthcare effectively.
Current trends indicate a heightened demand for mental health services, driven in part by evolving social dynamics and increased public awareness. A compelling case study could be the deployment of mental health first aid training across schools in Wales, which prioritises the mental well-being of young individuals. Concurrently, there is an urgent need to enhance chronic disease management programs, particularly as conditions like diabetes and heart disease continue to escalate.
Engaging healthcare professionals and incorporating community feedback can aid in identifying which services necessitate immediate enhancement. Striking a balance between expanding existing services and the urgent development of new ones is of paramount importance. The ongoing challenge lies not only in expanding services but ensuring they are equitable and accessible, which underscores the critical need for a meticulously crafted prioritisation strategy.
Significant Investment in Healthcare Infrastructure for Effective Scaling
The foundation of any successful healthcare scaling initiative is its infrastructure. Without adequate financial backing for new healthcare facilities and modern equipment, any efforts at expansion can quickly become untenable. The NHS’s infrastructure is ageing, making investment in modern facilities essential for scaling healthcare services effectively.
Consider the ambitious plans for the construction of new hospitals in the North East of England, designed to cater to a growing population and the increasing demand for healthcare services. Investment in digital infrastructure, including electronic health records and telemedicine capabilities, is equally critical. These technological advancements not only streamline operational processes but also enhance patient care, reinforcing the argument for additional investment.
However, the challenge extends beyond financial input; it demands a visionary approach. As healthcare demands evolve, so too must the facilities that support them. Innovative designs that prioritise patient-centric spaces can lead to improved health outcomes, demonstrating that investment in infrastructure is about creating environments conducive to healing rather than just physical structures.
Advocating strongly for infrastructure investment at the government level ensures that healthcare scaling is not left to chance. Collaborating with construction firms and technology companies can further enhance the delivery of effective healthcare services. The message is clear: without a progressive approach to infrastructure investment, the ability to scale healthcare services within the UK will continue to face significant hurdles.
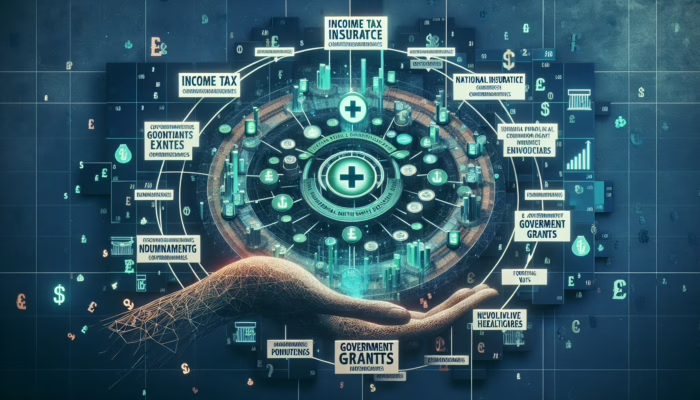
Strategic Distribution of Grants and Subsidies to Enhance Healthcare
Effectively allocating government and private grants can be transformative for enhancing healthcare services throughout the UK. The NHS, alongside various charitable organisations, has access to a multitude of funding opportunities that can be harnessed for scaling initiatives. However, the key to success lies in deploying these resources where they can yield the most substantial impact.
Take, for instance, the role of the Health Foundation and similar organisations that offer grants focused on specific service improvements. A recent initiative funded by a grant aimed at reducing waiting times in emergency departments in London has demonstrated promising results, underscoring the significance of targeted funding.
Moreover, understanding the intricacies of the grant application process and the criteria established by funding bodies can empower healthcare administrators to secure vital funds. Training sessions centred on grant writing and resource allocation can equip staff with the necessary skills to navigate this complex landscape. The potential for innovative projects, such as community health initiatives or mental health outreach programmes, hinges on the ability to effectively acquire and utilise these grants.
As we contemplate the future of healthcare in the UK, the strategic allocation of grants and subsidies must be regarded as an essential component of scaling efforts. Actively engaging stakeholders within the community can foster collaborative projects that resonate with the public, ultimately enhancing the overall health service ecosystem.
Long-term Financial Planning for Sustainable Healthcare Growth
Developing robust financial strategies is fundamental to ensuring the long-term viability and growth of the NHS. As healthcare demands evolve, so too must the financial strategies that underpin them. Strategic financial planning must consider not only immediate requirements but also future challenges that could impact healthcare delivery.
One effective method is scenario planning, where healthcare leaders forecast various financial scenarios based on current trends and potential shifts in policy or public health needs. This foresight prepares organisations to pivot swiftly in response to an evolving economic landscape. For instance, the financial adjustments necessitated by a pandemic exemplify the rapid changes required across the board.
Additionally, forming alliances with financial institutions can provide insights into sustainable investment practices that will benefit the NHS over the long term. Identifying alternative revenue streams, such as philanthropic donations or social enterprise models, can further bolster financial resilience.
There is an urgent need to demystify financial jargon for healthcare professionals who may lack a financial background. Workshops focused on budgeting, forecasting, and economic principles can empower staff to engage actively in the financial planning process. Ultimately, effective financial planning serves as the foundation upon which the future of healthcare scaling in the UK will be built, ensuring that services not only expand but also thrive sustainably.
Addressing Workforce Challenges in Healthcare Scaling
Combatting Staffing Shortages in the UK Healthcare System
The challenge of staffing shortages within the UK healthcare system is a pressing issue that cannot be overlooked. A well-trained workforce is crucial for effective healthcare scaling; however, many areas are currently experiencing acute shortages of healthcare professionals, from doctors to nurses. The chain of care is only as robust as its weakest link.
A glaring example of this problem can be observed in rural healthcare settings, where access to skilled professionals is often severely limited. Regions in Scotland, for instance, struggle to attract and retain medical staff, jeopardising the scalability of essential services. This challenge transcends mere recruitment; it involves ensuring that new hires are adequately trained and prepared to provide high-quality care.
Innovative strategies for workforce development are urgently needed. Initiatives such as accelerated training programmes for nurses or the implementation of international recruitment strategies could serve as interim solutions. Collaborations with universities to develop flexible degree pathways tailored to the needs of the NHS could also pave the way for future workforce sustainability.
Moreover, understanding workforce culture and cultivating an environment that promotes job satisfaction is paramount. Initiatives aimed at enhancing employee engagement and well-being can significantly reduce turnover rates, enabling healthcare systems to scale without the continuous burden of recruitment. The commitment to nurturing a resilient workforce is essential as the healthcare landscape continues to evolve.
Enhancing Training and Development for Healthcare Professionals
Training and development serve as the lifeblood of a responsive healthcare system. As services expand, so too do the demands placed on healthcare workers to adapt and evolve. It is insufficient to simply increase staffing numbers; healthcare professionals must also be equipped with the right skills to meet the challenges posed by a growing healthcare landscape.
The NHS has implemented a variety of training programmes aimed at upskilling the workforce, such as the NHS Leadership Academy, which focuses on cultivating future leaders within the healthcare sector. These initiatives underscore the importance of continuous professional development in effectively scaling healthcare services.
Furthermore, the integration of technology into training can significantly enhance learning outcomes. For instance, virtual reality training for scenarios such as emergency response or patient care can provide immersive experiences that traditional training methods lack. The incorporation of digital tools in training can lead to more competent, confident staff who are better prepared to meet the demands of an expanding patient population.
Additionally, prioritising diversity and inclusivity in training materials can foster a workforce capable of providing culturally competent care as services scale. Understanding the social determinants of health and the unique needs of diverse populations will ensure that the expansion of services is equitable and responsive to all citizens. As the complexities of healthcare continue to grow, so too must the approach to training and development.
Implementing Effective Retention Strategies for Healthcare Staff
In the context of scaling healthcare services, retaining skilled staff is just as crucial as recruitment. The costs associated with losing experienced professionals can have detrimental effects on service delivery and hinder expansion efforts. Therefore, implementing effective retention strategies is vital.
A study conducted by the King’s Fund highlighted that workplace culture and job satisfaction are significantly correlated with retention rates. Creating an environment where healthcare professionals feel valued and supported is essential. Initiatives that promote work-life balance, provide mental health support, and encourage professional development can contribute to a more supportive workplace culture.
Moreover, recognition and reward programmes that celebrate staff achievements can instil a sense of belonging and purpose. For example, the NHS Heroes campaign sought to acknowledge the extraordinary contributions of healthcare workers during the pandemic, reinforcing their value within the system.
Investing in career progression opportunities is another critical retention strategy. By providing clear pathways for advancement, healthcare organisations can motivate staff to remain within the system and grow alongside it.
As the NHS aims to scale its services, fostering a culture of appreciation and support will be pivotal in retaining talent. Ultimately, the challenge lies not just in attracting healthcare professionals but in creating an environment that encourages their continued presence and growth.
Navigating Regulatory and Compliance Issues in Healthcare Scaling
Ensuring Compliance with NHS Standards
In the pursuit of scaling healthcare services, compliance with NHS standards is an absolute necessity. The regulatory framework governing healthcare in the UK is designed to ensure safety, quality, and efficacy. However, as services expand, maintaining compliance can present significant challenges.
Healthcare providers must navigate a complex landscape of regulations that can vary greatly by region and service type. For instance, newly established clinics in urban areas must adhere to stringent accessibility requirements, guaranteeing that all patients, including those with disabilities, can access services without hindrance.
Moreover, compliance with NHS standards often involves regular inspections and audits to assess adherence. Preparing for these evaluations necessitates foresight and meticulous planning. Engaging a dedicated compliance officer or team can streamline processes and ensure ongoing adherence, allowing healthcare organisations to concentrate on delivering care rather than scrambling to meet regulatory demands.
The evolution of healthcare standards, particularly in light of rapid technological advancements, also poses challenges. For example, telehealth services require compliance with specific guidelines regarding patient confidentiality and data security. Staying informed about these changes is crucial for successful scaling, as non-compliance can lead to severe penalties.
Ultimately, a proactive approach to compliance not only safeguards patient safety but also strengthens public trust in the healthcare system. By embedding adherence into the organisational culture, healthcare providers can seize scaling opportunities while remaining committed to quality care.
Implementing Robust Quality Control Measures
As healthcare services expand, maintaining high standards of care becomes increasingly critical. Robust quality control measures are essential to ensure that scaling does not compromise patient safety or care outcomes.
One effective approach to ensuring quality is the implementation of evidence-based practices across all levels of service delivery. Standardising protocols and guidelines can help maintain consistency, whether in a bustling metropolitan hospital or a rural health clinic. For instance, the introduction of standard operating procedures for managing chronic diseases can ensure that patients receive uniform care, regardless of their location.
Regular audits and feedback mechanisms are vital components of quality control. Collecting data from patient satisfaction surveys can provide invaluable insights into areas that require improvement. Engaging healthcare workers in this process fosters a culture of continuous improvement, enabling staff to identify and address issues promptly.
Moreover, incorporating patient feedback into the scaling process highlights the importance of patient-centred care. Systems that allow patients to share their experiences and outcomes can drive enhancements in service delivery.
Quality control measures are not merely a regulatory requirement; they are the foundation upon which trust in the healthcare system is built. Ensuring that scaling efforts do not compromise these standards is vital for the future of healthcare in the UK.
Safeguarding Data Protection and Privacy in Healthcare
In today’s era, where data breaches are alarmingly frequent, safeguarding patient data is of utmost importance. As healthcare services scale, the complexities surrounding data protection and privacy multiply. The NHS must navigate stringent regulations, such as the General Data Protection Regulation (GDPR), to ensure that patient information is handled with the utmost care.
Implementing robust data protection protocols is essential. This includes educating all staff members about their responsibilities regarding the handling of sensitive patient information. Regular training sessions can ensure that everyone understands the significance of privacy and the potential repercussions of non-compliance.
Moreover, as the prevalence of telehealth services increases, the need for secure communication channels becomes increasingly critical. Utilising encrypted communication tools can protect patient data from cyber threats while still facilitating efficient service delivery.
Establishing a designated data protection officer can further streamline compliance efforts. This individual can oversee data management practices, ensuring that all protocols align with legal requirements and best practices.
Proactively addressing data protection and privacy issues will not only prevent breaches but also foster trust among patients. As healthcare providers scale their services, a strong commitment to safeguarding patient information must remain at the forefront of their initiatives.
Enhancing Regulatory Reporting and Audit Processes
Timely and accurate regulatory reporting serves as a cornerstone of compliance within the healthcare sector. As services expand, the complexity of these reports can become overwhelming, making it imperative for healthcare organisations to develop efficient processes for regulatory compliance.
Regular audits are an integral part of the healthcare landscape, ensuring that organisations adhere to established standards. Preparing for these audits requires diligent record-keeping and a comprehensive understanding of the relevant regulations. Establishing a robust reporting framework can streamline this process, enabling healthcare providers to focus on patient care rather than administrative burdens.
Furthermore, leveraging technology can enhance the efficiency of reporting processes. Implementing electronic health record systems that facilitate real-time data collection can provide auditors with immediate access to essential information. This not only simplifies the audit process but also enhances data integrity.
Incorporating lessons learned from previous audits can lead to meaningful improvements in practice. By fostering a culture of transparency and accountability, healthcare organisations can approach audits not as a chore but as an opportunity for growth and refinement.
Ultimately, embracing regulatory reporting as a critical aspect of operational excellence will enable healthcare providers to scale confidently, knowing they are compliant and ready to meet the expectations of regulators and the public alike.
Technological Integration as a Key to Healthcare Scaling
Embracing Digital Tools for Enhanced Healthcare Delivery
In an era characterised by rapid advancement, the adoption of digital tools in healthcare is not merely advantageous; it is essential. The UK’s healthcare landscape is undergoing a significant transformation, with technology paving the way for improved patient outcomes and operational efficiency. As services scale, the integration of innovative digital solutions becomes a top priority.
Telemedicine represents a monumental leap forward in healthcare delivery. By leveraging video conferencing tools, healthcare providers can offer consultations to patients who may have difficulty travelling. This is particularly beneficial for individuals in remote areas of Scotland, where access to specialists can be limited.
Moreover, the adoption of electronic health records (EHR) significantly enhances the quality of care. EHR systems facilitate seamless data sharing among healthcare providers, ensuring that patient information is readily available when needed. This integration can drastically reduce errors and improve care coordination, making it a vital component of scaling healthcare services.
However, the transition to digital tools must be managed with care. Staff training is critical to ensure that all healthcare professionals are comfortable using new technologies. Implementing change management strategies can ease the transition and foster a culture of innovation within healthcare organisations.
Ultimately, the successful adoption of digital tools is not solely about efficiency; it is about elevating the standard of care. As the UK healthcare system scales, embracing technology will play a pivotal role in shaping its future.
Tackling Interoperability Challenges in Healthcare Systems
As healthcare systems become increasingly intricate, interoperability challenges emerge. Ensuring that different healthcare systems can communicate effectively is crucial for providing seamless care. The absence of interoperability can result in significant barriers, especially as services scale across various regions.
In the UK, the integration of different EHR systems poses a major obstacle. For instance, when a patient visits multiple healthcare providers, their medical history may not be readily accessible, leading to fragmented care. Bridging these gaps necessitates collaborative efforts among healthcare organisations to standardise data-sharing protocols.
Innovative solutions, such as health information exchanges (HIEs), can facilitate interoperability. These platforms enable the secure exchange of patient data across different systems, ensuring that healthcare providers have the necessary information at their fingertips. By promoting interoperability, we can enhance care coordination and ultimately improve patient outcomes.
Moreover, engaging stakeholders in the development of interoperability standards is crucial. By involving healthcare professionals, IT specialists, and policymakers, we can create a cohesive framework that addresses the unique needs of the UK’s healthcare system.
As we look towards the future, addressing interoperability challenges will be vital for the successful scaling of healthcare services. A commitment to seamless communication will not only enhance efficiency but also elevate the standard of patient care.
Addressing Cybersecurity Concerns in Healthcare
In the age of digital transformation, concerns surrounding cybersecurity are ever-present. As healthcare scales and adopts more technology, the risk of cyber threats escalates. Protecting sensitive patient data is paramount; thus, healthcare organisations must take proactive steps to safeguard against potential breaches.
The NHS has encountered cyberattacks in the past, underscoring the vulnerabilities within the system. To mitigate these risks, healthcare providers must invest in robust cybersecurity measures. This includes implementing advanced encryption protocols, conducting regular security audits, and training staff to identify potential threats.
Moreover, cultivating a culture of cybersecurity awareness is critical. Engaging staff in discussions about data protection can foster vigilance against cyber threats. Workshops and training sessions can empower employees to recognise phishing attempts and other common attacks.
Additionally, collaborating with cybersecurity experts can provide valuable insights into emerging threats and best practices for protection. As technology continues to evolve, so too must our strategies for safeguarding patient data.
Ultimately, addressing cybersecurity concerns is not just a technical necessity; it is a matter of public trust. As healthcare services expand, a commitment to data protection will ensure that patients feel secure in the care they receive.
Ensuring Patient Access and Equity in Healthcare Scaling
Confronting Geographical Disparities in Healthcare Access
The geographical disparities in healthcare access across the UK present formidable challenges as services scale. While urban areas may enjoy an abundance of healthcare resources, rural regions often face stark limitations. Addressing these disparities is critical for ensuring that all citizens receive equitable care.
For instance, a patient residing in a remote part of Wales may need to travel considerable distances to access specialist services. This not only presents logistical challenges but can also result in delays in treatment. As healthcare scales, innovative solutions must be sought to bridge these gaps.
Mobile healthcare units have emerged as a promising strategy for reaching underserved populations. These units can provide essential services, such as vaccinations and health screenings, directly to communities in need. By bringing healthcare to the patients, we can mitigate the barriers posed by geographical distance.
Furthermore, telehealth services can play a vital role in improving access for rural populations. By leveraging technology, healthcare providers can connect with patients virtually, offering consultations that eliminate the need for travel. This is particularly beneficial for mental health services, where stigma and distance often deter individuals from seeking care.
Ultimately, addressing geographical disparities is not merely a logistical concern; it is a matter of health equity. As healthcare services expand, ensuring equitable access must remain a priority in our efforts.
Mitigating Socioeconomic Barriers to Healthcare Access
Socioeconomic factors significantly influence healthcare access and outcomes. As we scale healthcare services, it is essential to consider how these variables affect different populations across the UK. Ensuring that scaling efforts benefit all socioeconomic groups is crucial for fostering a just healthcare system.
Individuals from lower socioeconomic backgrounds often encounter barriers to accessing healthcare. These may include financial constraints, lack of transportation, or limited health literacy. To address these challenges, healthcare providers must implement targeted initiatives aimed at alleviating these barriers.
For example, community health programmes that provide education on preventive care can empower individuals to take charge of their health. Additionally, partnerships with local organisations can enhance outreach efforts, ensuring that vulnerable populations are informed about available services.
Moreover, offering sliding-scale fees or free services can alleviate the financial burden on low-income patients. Initiatives like NHS Health Checks can provide essential health assessments at no cost, underscoring the importance of accessibility in scaling healthcare services.
Ultimately, recognising and addressing socioeconomic factors is critical for promoting health equity as we scale. By ensuring that our services are inclusive and accessible to all demographics, we can build a more equitable healthcare system that leaves no one behind.
Enhancing Cultural Competency in Healthcare Delivery
As healthcare services expand, providing culturally sensitive care becomes increasingly important. The UK is home to a diverse population, and understanding the cultural nuances of patients is essential for delivering effective services.
Culturally competent care involves recognising and respecting the unique backgrounds and beliefs of patients. Training healthcare professionals in cultural competency can enhance communication and foster trust between providers and patients. For instance, understanding dietary restrictions based on cultural practices can significantly improve patient satisfaction and adherence to treatment plans.
Moreover, engaging community leaders and representatives can provide valuable insights into the specific needs of diverse populations. Collaborating with local organisations can enhance outreach efforts and ensure services are tailored to meet the cultural preferences of patients.
Additionally, promoting diversity within the healthcare workforce can contribute to improved cultural competency. A workforce that reflects the community it serves is better equipped to understand and address the unique needs of patients from various backgrounds.
Ultimately, as healthcare services scale, a commitment to cultural competency will enhance patient experiences and outcomes. By embracing diversity and fostering understanding, we can create a healthcare system that respects and values every individual.
Innovating Service Delivery Models for Effective Healthcare Scaling
Implementing Integrated Care Systems for Seamless Service Delivery
The shift towards integrated care systems (ICS) signifies a transformative approach to the delivery of healthcare services in the UK. By fostering collaboration among healthcare providers, ICS aims to create a seamless experience for patients, which is crucial as services scale.
Integrated care systems facilitate communication between hospitals, general practitioners, and community services, ensuring that patients receive coordinated care throughout their healthcare journey. For instance, a patient with a chronic illness can benefit from a multidisciplinary team that collaborates to manage their care more effectively.
Moreover, ICS can address health inequalities by ensuring that services are tailored to meet the specific needs of diverse populations. Actively engaging local communities in the design and delivery of services promotes inclusivity and responsiveness, essential aspects of effective healthcare scaling.
The adoption of technology within integrated care systems also enhances service delivery. Shared electronic health records enable healthcare providers to access patient information in real time, fostering better decision-making and care coordination.
As integrated care systems continue to evolve, they hold great promise for transforming the UK healthcare landscape. By prioritising collaboration and patient-centred approaches, we can build a more efficient and effective healthcare system.
Expanding Telehealth Services for Enhanced Access
The expansion of telehealth services presents a significant opportunity for scaling healthcare in the UK. By harnessing digital technology, healthcare providers can reach patients who may otherwise face barriers to accessing care.
Telehealth offers a practical solution for addressing the challenges posed by geographical disparities. For instance, patients in rural areas can access specialist consultations without the need for extensive travel. This not only saves time but also reduces the burden on healthcare facilities.
Moreover, telehealth can enhance patient engagement and satisfaction. By providing convenience and flexibility, patients are more likely to seek care and adhere to treatment plans. Innovative platforms that facilitate remote monitoring of chronic conditions can further improve patient outcomes.
However, scaling telehealth services requires careful consideration of accessibility and equity. Ensuring that all patients have access to the necessary technology and internet connectivity is crucial for successful implementation.
Ultimately, the expansion of telehealth services has the potential to revolutionise healthcare delivery in the UK. By embracing this technology, we can create a more responsive and accessible healthcare system for all.
Advancing Community-Based Care Models
Enhancing local healthcare services through community-based care models is essential for addressing the specific needs of populations as healthcare scales. By concentrating on preventive care and early intervention, community-based care can improve health outcomes and alleviate pressure on acute services.
Community health initiatives, such as mobile clinics or health fairs, can reach underserved populations and provide essential services in familiar settings. For example, initiatives targeting maternal and child health can offer vital resources and support to families in need.
Moreover, engaging local health workers and community leaders in the delivery of care fosters trust and improves health literacy. By employing individuals who understand the cultural context of their communities, healthcare providers can create more effective outreach strategies.
Investing in training for community health workers empowers them to play a pivotal role in scaling healthcare services. These professionals can facilitate access to services, provide education, and support patients in navigating the healthcare system.
Ultimately, prioritising community-based care is vital for creating a resilient healthcare system. By addressing the unique needs of populations and fostering local engagement, we can ensure that scaling efforts are meaningful and impactful.
Building Public Perception and Trust in Healthcare Scaling
Developing Effective Communication Strategies
Implementing effective communication strategies is crucial for garnering public support and trust as healthcare services scale. In an era characterised by information overload, clarity and transparency become essential for engaging the public and ensuring they understand the changes taking place.
Healthcare organisations must proactively inform the public about scaling initiatives, highlighting both the benefits and addressing any concerns. Utilising social media platforms and community outreach can enhance engagement and foster a sense of involvement. For instance, running informative campaigns about new services or facilities can demystify changes and encourage community participation.
Moreover, tailoring messages to resonate with specific demographics is vital. Understanding the diverse needs of the population allows healthcare providers to communicate effectively, ensuring that messages are inclusive and relevant.
Additionally, providing regular updates on progress and outcomes can build trust over time. Transparency in decision-making processes and the rationale behind scaling efforts can further cultivate a positive public perception.
Ultimately, strategic communication is not merely about conveying information; it is about fostering a collaborative relationship with the public. As healthcare services scale, effective communication will be key to maintaining trust and support.
Managing Public Expectations During Healthcare Expansion
Aligning public expectations with the realities of healthcare expansion presents a critical challenge. As services scale, it is essential to provide realistic timelines and outcomes to avoid disappointment and frustration among patients and communities.
Managing expectations begins with clear communication. Setting the stage for what patients can realistically expect from new services or facilities can help mitigate potential backlash. For example, if a new urgent care centre is planned, communicating potential waiting times and services offered can effectively manage expectations.
Moreover, engaging with the community during the planning phase can provide valuable insights. Public forums and consultations can help healthcare providers gauge community needs and preferences, creating a sense of ownership in the scaling process.
Additionally, addressing concerns and feedback in real time demonstrates responsiveness and accountability. By being transparent about challenges and setbacks, healthcare organisations can cultivate a trusting relationship with the public, ultimately leading to a more supportive environment for scaling initiatives.
In an ever-evolving healthcare landscape, managing expectations is vital for ensuring public satisfaction and confidence. By fostering open dialogue and establishing realistic goals, healthcare providers can navigate the complexities of scaling with greater ease.
Establishing Trust in Newly Scaled Healthcare Services
Building public trust in newly scaled healthcare services is paramount for ensuring their success. As services expand, healthcare organisations must engage in proactive efforts to establish credibility and confidence among patients and communities.
Transparency plays a significant role in fostering trust. Clearly communicating the rationale behind new services, along with the evidence that supports their implementation, can reassure the public. For instance, sharing success stories from pilot programmes can demonstrate the effectiveness of new initiatives.
Moreover, involving healthcare professionals in the conversation can enhance credibility. Patients are more likely to trust services when they hear directly from providers about their experiences and the benefits of new care models. Hosting events where healthcare professionals interact with the community can create opportunities for dialogue and connection.
Additionally, incorporating patient feedback mechanisms can empower individuals to share their experiences with new services. By actively soliciting input and addressing concerns, healthcare organisations can demonstrate their commitment to patient-centred care.
Ultimately, building trust in new services requires ongoing effort and dedication. By fostering transparency, engaging stakeholders, and prioritising patient feedback, healthcare providers can cultivate a culture of trust as they scale services.
Promoting Transparency in Healthcare Operations
Encouraging transparency in healthcare operations is essential for enhancing public trust. As services scale, openness regarding processes, decisions, and outcomes fosters a sense of collaboration and accountability among patients and communities.
Healthcare organisations must adopt practices that encourage transparency. This includes providing clear information about service delivery, financial management, and decision-making processes. For instance, publishing performance metrics and patient satisfaction data can demonstrate a commitment to accountability.
Moreover, engaging with the public through community forums and open houses can create opportunities for dialogue. Inviting feedback and questions can empower individuals to feel involved and informed about the healthcare services available to them.
Additionally, fostering a culture of transparency among staff is vital. Encouraging open communication and collaboration within healthcare teams can enhance the quality of care delivered to patients. When staff members feel empowered to voice concerns or suggestions, it ultimately benefits the entire organisation.
In an era where trust in institutions is being tested, transparency in healthcare operations is more important than ever. By prioritising openness and accountability, healthcare providers can cultivate trust and support as they scale services.
Engaging Communities in Healthcare Planning
Involving local communities in healthcare planning is crucial for fostering trust and ensuring services meet public needs. Community engagement initiatives create a platform for collaboration and dialogue, allowing healthcare providers to better understand the unique requirements of the populations they serve.
Healthcare organisations can implement community advisory boards that include diverse voices from the community. These boards can provide valuable insights into local health needs, preferences, and concerns, guiding decision-making as services scale.
Moreover, hosting community events and workshops can create opportunities for engagement. By facilitating discussions around new initiatives and soliciting feedback, healthcare providers can demonstrate their commitment to serving the community’s interests.
Additionally, leveraging partnerships with local organisations can enhance outreach efforts. Collaborating with schools, faith-based organisations, and community groups can strengthen connections and build trust.
Ultimately, community engagement is not a one-time event but an ongoing process. By involving the public in healthcare planning and decision-making, providers can create a more responsive and inclusive healthcare system that meets the diverse needs of the population.
Implementing Monitoring and Evaluation Systems for Healthcare Scaling
Establishing Clear Performance Metrics for Success
Establishing clear performance metrics is fundamental to measuring the success of healthcare scaling efforts. These metrics provide quantifiable data that can inform decision-making and guide improvements, ensuring that services evolve to meet the needs of patients effectively.
Healthcare organisations must identify key performance indicators (KPIs) that align with their goals for scaling. For example, metrics related to patient outcomes, service utilisation rates, and patient satisfaction can provide valuable insights into the impact of new services.
Regularly reviewing performance metrics allows healthcare providers to track progress and identify areas for improvement. By analysing trends over time, organisations can make data-driven decisions that enhance service delivery.
Moreover, engaging staff in the development of performance metrics fosters a sense of ownership and accountability. When healthcare professionals understand how their contributions impact overall performance, they are more likely to be invested in achieving positive outcomes.
Ultimately, effective monitoring and evaluation of performance metrics are crucial for ensuring that scaling efforts are successful. By leveraging data to inform decisions, healthcare providers can create a more responsive and effective healthcare system.
Incorporating Feedback Mechanisms for Continuous Improvement
Integrating patient and staff feedback into scaling efforts is essential for continuous improvement. Feedback mechanisms provide valuable insights that can guide adjustments and enhance the overall quality of care.
Establishing formal feedback channels, such as surveys or suggestion boxes, can empower patients and staff to voice their opinions. For example, conducting patient satisfaction surveys after new services are implemented can provide immediate insights into what’s working and what needs refinement.
Moreover, creating forums for open dialogue between staff and management encourages a culture of transparency and collaboration. Regularly scheduled meetings or focus groups can facilitate discussions around challenges and successes, allowing for collective problem-solving.
Additionally, responding to feedback is crucial for building trust. When patients and staff see that their input leads to tangible changes, it fosters a sense of ownership and commitment to the organisation.
Ultimately, effective feedback mechanisms are an integral part of the scaling process. By valuing and acting on input from patients and staff, healthcare providers can enhance service delivery and patient satisfaction.
Fostering Continuous Improvement in Healthcare Services
The journey of scaling healthcare services is not a one-time event; it is an ongoing process of continuous improvement. Embracing a culture of learning and adaptation is essential for ensuring that services evolve to meet changing patient needs effectively.
Healthcare organisations must cultivate an environment that encourages innovation and experimentation. For instance, pilot programmes for new services can provide valuable insights into what works and what doesn’t, allowing organisations to refine their approaches before full-scale implementation.
Moreover, investing in staff training and development fosters a culture of continuous improvement. By equipping healthcare professionals with the skills and knowledge needed to adapt to new challenges, organisations can enhance their capacity for scaling.
Engaging in regular evaluations of current practices is also critical. Healthcare organisations should assess their processes and outcomes to identify areas for improvement continually. This commitment to reflection and adaptation ensures that scaling efforts are responsive to the evolving healthcare landscape.
Ultimately, a mindset of continuous improvement is essential for achieving success in scaling healthcare services. By prioritising learning and adaptation, healthcare providers can create a more effective and sustainable system.
Utilising Data Analysis and Reporting for Informed Decision-Making
Analysing collected data and generating reports is vital for informing decision-making and tracking progress in healthcare scaling initiatives. Data analysis provides insights that can guide resource allocation, service delivery, and overall performance.
Healthcare organisations must establish robust data management systems that facilitate the collection and analysis of relevant information. By leveraging technology, organisations can streamline data collection processes and ensure accuracy.
Regular reporting on key metrics can provide stakeholders with a clear picture of progress. For instance, sharing data on patient outcomes, service utilisation rates, and patient satisfaction can highlight successes and areas for improvement.
Moreover, engaging stakeholders in the data analysis process fosters transparency and collaboration. By involving staff in discussions around data findings, organisations can harness collective insights to drive improvements.
Ultimately, effective data analysis and reporting are central to the success of healthcare scaling initiatives. By leveraging data to inform decisions, healthcare providers can create a more responsive and effective system.
Building Collaborative Partnerships for Healthcare Scaling
Harnessing Public-Private Partnerships for Enhanced Healthcare Services
Leveraging public-private partnerships (PPPs) can be a transformative strategy for scaling healthcare services in the UK. By collaborating with private organisations, healthcare providers can access additional resources, expertise, and innovative solutions that enhance service delivery.
PPPs can take various forms, from joint ventures to contract partnerships. For instance, collaborations with technology firms can facilitate the integration of digital tools that improve patient care and operational efficiency. In one notable example, partnerships between the NHS and tech companies have resulted in the development of mobile health applications that empower patients to manage their health proactively.
Moreover, engaging private sector investments can bolster infrastructure development. The construction of new healthcare facilities or the expansion of existing ones can be significantly expedited through collaborative efforts, enabling healthcare organisations to meet increasing demands more swiftly.
However, successful public-private partnerships require careful planning and alignment of goals. Establishing clear expectations and accountability measures is vital to ensure that all parties are working towards common objectives. Additionally, transparency in financial arrangements fosters trust and collaboration.
Ultimately, public-private partnerships hold great promise for scaling healthcare services in the UK. By harnessing the strengths of both sectors, healthcare providers can create a more efficient and effective system that meets the needs of the population.
Fostering Inter-agency Cooperation for Comprehensive Healthcare Solutions
Collaboration among various government agencies is essential for supporting healthcare expansion efforts. Inter-agency cooperation can create synergies that enhance the effectiveness of scaling initiatives and ensure that services are responsive to the needs of diverse populations.
For example, partnerships between health departments and local councils can facilitate the delivery of integrated services that address social determinants of health. By working together, agencies can develop programmes that promote health equity and access to care.
Moreover, engaging with educational institutions can create pathways for workforce development. Collaborative initiatives that focus on training and internships can ensure that future healthcare professionals are equipped to meet the challenges of an evolving healthcare landscape.
Additionally, inter-agency cooperation can enhance data sharing and coordination of services. By establishing common protocols for data exchange, agencies can create a holistic view of patient needs and outcomes, leading to improved care coordination.
Ultimately, fostering inter-agency cooperation is crucial for scaling healthcare services effectively. By leveraging the strengths of various organisations, healthcare providers can create a more integrated and responsive system that meets the diverse needs of the population.
Engaging Communities for Effective Healthcare Solutions
Involving local communities in the scaling process is essential for ensuring that services are relevant and impactful. Community engagement initiatives create opportunities for collaboration and dialogue, allowing healthcare providers to better understand the unique needs of the populations they serve.
Healthcare organisations can implement community advisory boards that include a diverse array of voices. These boards can provide valuable insights into local health needs, preferences, and concerns, guiding decision-making as services scale.
Moreover, hosting community events and workshops can create opportunities for engagement. By facilitating discussions around new initiatives and soliciting feedback, healthcare providers can demonstrate their commitment to serving the community’s interests.
Additionally, leveraging partnerships with local organisations can enhance outreach efforts. Collaborating with schools, faith-based organisations, and community groups can strengthen connections and build trust.
Ultimately, community engagement is not a one-time event but an ongoing process. By involving the public in healthcare planning and decision-making, providers can create a more responsive and inclusive healthcare system that meets the diverse needs of the population.
FAQs about Scaling Healthcare Services
What are the primary challenges in scaling healthcare services?
The primary challenges in scaling healthcare services encompass funding and resource allocation, staffing shortages, regulatory compliance, and ensuring equitable access. Addressing these challenges is essential for successful expansion.
How can healthcare organisations enhance funding allocation?
Healthcare organisations can enhance funding allocation by prioritising services based on community needs, exploring public-private partnerships, and securing grants that target specific health initiatives.
What role do digital tools play in healthcare scaling?
Digital tools enhance healthcare scaling by improving operational efficiency, enabling remote consultations, and facilitating data sharing among providers. They also empower patients to take an active role in managing their health.
How can organisations ensure patient access and equity?
To ensure patient access and equity, organisations must address geographical disparities, engage with underserved populations, and implement culturally competent care practices.
What are effective strategies for retaining healthcare staff?
Effective strategies for retaining healthcare staff include creating a supportive workplace culture, offering career development opportunities, and implementing recognition programmes that acknowledge staff contributions.
Why is community engagement vital in healthcare scaling?
Community engagement is crucial in healthcare scaling as it ensures that services align with local needs, fosters trust, and encourages collaboration between healthcare providers and the public.
What is the significance of performance metrics in healthcare?
Performance metrics are significant as they provide quantifiable data that informs decision-making, tracks progress, and identifies areas for improvement in healthcare services.
How can healthcare organisations manage public expectations during scaling?
Healthcare organisations can manage public expectations by communicating transparently about new services, setting realistic timelines, and involving the community in the decision-making process.
What benefits do public-private partnerships offer in healthcare?
Public-private partnerships offer benefits such as access to additional resources, expertise, and innovative solutions that enhance service delivery and improve patient outcomes.
How can healthcare providers maintain compliance with regulations during scaling?
Healthcare providers can maintain compliance by establishing clear processes for regulatory reporting, conducting regular audits, and engaging compliance officers to oversee operations.
The post Healthcare Scaling Pitfalls: Navigating Key Challenges appeared first on Healthcare Marketing Service.